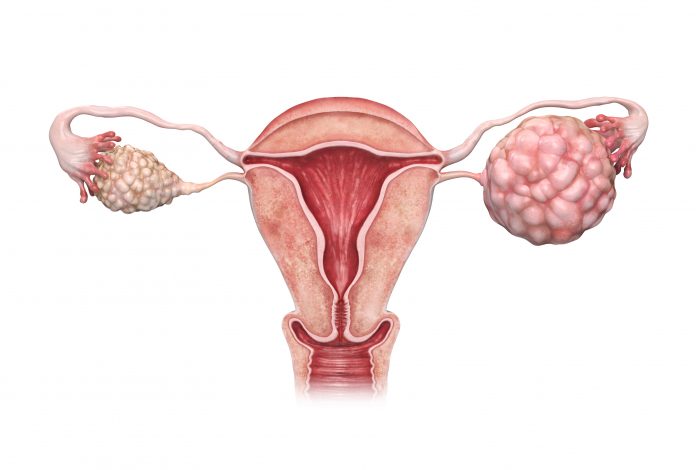
Scientists from the University of California (UC), San Diego, and their collaborators have demonstrated how key proteins act together to suppress antitumor activity in high-grade serous ovarian carcinoma (HGSOC) in a mouse model, revealing a new combinatorial strategy to treat this intractable malignancy.
Hallmarks of a lethal form of ovarian cancer, HGSOC, are an immunosuppressive tumor microenvironment, insensitivity to checkpoint inhibitor immunotherapies, and elevated expression of checkpoint pathway ligands that thwart the immune system’s ability to kill tumor cells. Nearly 70% of HGSOC tumors express PTK2, a gene that encodes FAK (focal adhesion kinase), elevated levels of which signal poor survival outcomes.
In a study published in the journal Proceedings of the National Academy of Sciences, scientists show how this type of cancer can be targeted.
“Ovarian cancer is one of oncology’s greatest challenges,” said David Schlaepfer, a professor in the department of obstetrics, gynecology, and reproductive sciences at UC San Diego School of Medicine and senior author of the study. “Tumors can develop without obvious symptoms. The most common sign of ovarian cancer is abdominal swelling when the disease is advanced, which is when most women are diagnosed.”
Ovarian cancer is the fifth leading cause of cancer deaths among women and the majority of these cases are HGSOC tumors, according to the American Cancer Society.
Using transcriptomic analysis of ovarian cancer databases, an aggressive mouse ovarian tumor model, and multiplex immunofluorescence assays, the researchers demonstrated that FAK activation regulates CD155 expression, which is a checkpoint ligand for a T cell immunoreceptor called TIGIT. Based on this mechanistic discovery they found that combining an oral FAK inhibitor and a TIGIT antibody that blocks the immunoreceptor’s function, generated a significant antitumor response and increased survival time of a mouse model of the lethal cancer.
“In HGSOC tumors, where high levels of CD155 and active FAK are common, our results provide compelling support for targeting FAK and TIGIT as part of a new immune-boosting therapeutic strategy,” said Schlaepfer.
Immunotherapy is a treatment strategy that uses a person’s own immune cells to fight malignancy and has been successfully used to treat a variety of cancers, but it has not been effective in treating HGSOC.
![FAK (in green) makes tumors more malignant by binding to immune-regulating protein, CD155 (in red) and preventing CD3 expressing T cells (in magenta) from infiltrating the tumor. [UC San Diego Health Sciences]](https://www.clearityfoundation.org/wp-content/uploads/2022/04/2022_04_11_ovarian-cancer-schlaepfer-300x300.jpg)
Lead author of this study, Duygu Ozmadenci, a postdoctoral researcher in Schlaepfer’s lab, and his collaborators showed that active, phosphorylated FAK increased in late-stage HGSOC tumors and colocalized with CD155 in HGSOC tumors. They also showed HGSOC tumors with high FAK expression expressed low levels of CD3 transcripts that mark T cells that tumor infiltrate tumors.
An analysis of a patient transcriptomic database, and in vitro and in vivo experiments supported a selective binding between FAK and TIGIT checkpoint ligands. Through high levels of CD155, the tumor builds a safe environment for cancer cells to grow and evade immune detection and attack.
The researchers treated a mouse model of ovarian cancer with an oral anti-FAK drug and demonstrated reduced CD155 and other checkpoint proteins.
“We used a newly derived murine tumor model termed KMF (Kras, Myc, FAK amplified) as an aggressive platinum-resistant tumor model in immune-competent mice to show that genetic or pharmacological FAK inhibition resulted in the recruitment and activation of T cells,” said Schlaepfer.
In combination with a TIGIT-blocking antibody, the oral anti-FAK drug resulted in immune cell activation and tertiary lymphoid structure formation that mark a positive antitumor immune response. This in turn resulted in smaller tumors and prolonged survival of the mouse model.
Schlaepfer noted that several companies are testing FAK inhibitors and TIGIT immunotherapy, while this study provides the rationale for a combined immunotherapy. Schlaepfer’s team intends to conduct clinical trials of oral FAK inhibitors with anti-TIGIT blocking antibodies. He said, “Translational studies incorporating the testing of putative biomarkers are not only logical, but also feasible given the combinatorial potential of FAK inhibitors and antibody therapies targeting the CD155/TIGIT axis currently in clinical trials.”
This article was published by Inside Precision Medicine.